Mobile
Hospital Air Purification
Equipment Systems for Airborne Infection Control Diseases TB Tuberculosis
Mobile Negative Pressure Isolation Rooms TB Tuberculosis
|
MICROCON® 800 & 400 Mobile Negative Pressure Isolation Room TB Tuberculosis
all Units with HEPA Filtration and optional Germicidal Ultra Violet UV Irradiation for Hospital and Health Care
Mobile Airborne Infection Control - Air Purification Systems
|
|
Biological Controls' Mobile Hospital Airborne Infection Control for TB Tuberculosis
MICROCON ® 800/400 HEPA Filter Units Over 4,000 Unit Installations in Hospitals, Worldwide. Including Health Care Facilities, Centers and Clinics throughout the US.
The MICROCON 800/400 HEPA Filter hospital and healthcare units create Mobile Negative Air Pressure Isolation Rooms for the treatment of Tuberculosis TB in Hospital Isolation Rooms and Positive Air Pressure for Bone Marrow Transplants and HIV patients.
Meeting all CDC Guidelines 100% for Hospital Airborne Infection Control and Health Care Facilities (Healthcare). MICROCON® "The only patented mobile hospital air purification system specifically designed for removal of airborne contaminants in Hospitals and Health Care (Healthcare) settings." All of our Air Purification HEPA filter units comply with CDC Guidelines, and are FDA 510K certified. “An FDA 510K certification is mandatory for air purification systems in hospital use!”
Features for Airborne Infection Control in Hospitals and Health Care Facilities, Healthcare Clinics and Healthcare Centers:
 360° Air intake and exhaust 360° Air intake and exhaust
 Air change capacity Air change capacity
 Breathing zone filtration Breathing zone filtration
 Certified HEPA filtration Certified HEPA filtration
 Portability Modular design Portability Modular design
 Safe filter replacement Safe filter replacement
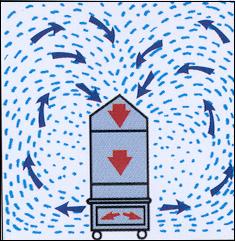
The MICROCON® is a high capacity mobile air purifier specifically designed to remove hazardous microbial airborne particulate. It is the only system available that offers our unique CIRCUMFLOW ® air distribution pattern. This is created by the 360-degree air intake and exhaust, which are unique only to the MICROCON® series. No other competitive units replicate this feature, which has been documented, to greatly improve "Breathing Zone Filtration" within a room.
It is available in two models, the MICROCON® 800 and 400. Either meets the CDC requirements for HEPA filtration and exceeds CDC recommendations 6 to 12 room air changes per hour. Each unit is portable and can be positioned for spot or more permanent applications. It does not restrict room use since it's not a permanent installation, allowing you flexibility on planning patient load.
Four-254 nm Germicidal Ultraviolet (Ultra Violet) Lamps are available on either model. Lamp life expectancy is rated at 6000 hours. Positioned downstream of the HEPA, they are fully shielded and eliminate the maintenance requirements of competitive units when UV bulbs are directly in the air stream attracting dust particulate to bulb surface and diminishing irradiation. An electronic sensor bar, to continually monitor bulb malfunction, and hour meter, to register system operation time, are available. See our HEPA Filter Replacement Guidelines in Product Details below.

MICROCON® 800 MUV (with
filter cube removed)
|

MICROCON® 400 & 800
| Breathing
Zone Filtration for Airborne Infection Control |
The MICROCON® intakes air from the top of the unit in a 360 degree direction from within the "breathing zone". This zone measures anywhere from 3 ft. to 7 ft. from the floor level. Eliminating sub micron-size infectious airborne particles from this zone reduces airborne microbial migration and the risk of inhalation.
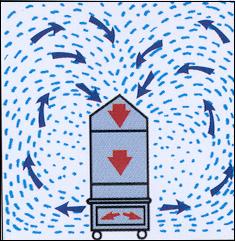
CIRCUMFLOW® Air Distribution Pattern 
|
|
|
|
Create a Negative or Positive pressure room with the MICROCON® 800 by adding various attachments.
The MICROCON® 800 is designed to create a variety of air purification and pressurization applications. The unique design of the original unit as an in-room filtration device for increasing air changes also lends itself to providing a negative or positive pressure environment. Additional components can be installed to redirect the airflow and bring in air from outside the room when positive pressurization is required. Or by attaching an exhaust duct to the base and expelling air to the outside of the room thereby creating a negative pressure room. All components are simply attached to pre-threaded fasteners in the base or cap for a quick and easy conversion based upon your patient's changing needs.

MICROCON® 800MUV equipped
for in-room re-circulationClick here for schematics
to create MICROCON® pressure differential options
|

MICROCON® 800MUV equipped
to provide exhaust for
negative pressureClick here for schematics
to create MICROCON® pressure differential options
|

Same unit as on left, but side
view showing rear exhaustClick here for schematics
to create MICROCON® pressure differential options
|

MICROCON® 800MUV with
inlet for creating positive pressure Click here for schematic of
creating positive pressure
with the MICROCON® 800
|
| Product
Details (click link) |
|
Glossary Section below for definitions and requirements thereof:
What is Airborne Disease
About Airborne Disease
Airflow and Ventilation Procedures
Glossary:
What is airborne disease.
Airborne diseases include any that are caused by pathogens and transmitted through the air. Some are of great medical importance. The pathogens transmitted may be any kind of microbe, and they may be spread in aerosols of dust or liquids. The aerosols might be generated from sources of infection such as the bodily secretions of an infected animal or person, or biological wastes such as accumulate in lofts, caves, garbage and the like. Such infected aerosols may stay suspended in air currents long enough to travel for considerable distances on air currents, though the rate of infection decreases sharply with the distance between the source and the organism infected. Airborne pathogens or allergens often cause inflammation in the nose, throat, sinuses and the lungs. This is caused by the inhalation of these pathogens that affect a person's respiratory system or even the rest of the body. Sinus congestion, coughing and sore throats are examples of inflammation of the upper respiratory air way due to these airborne agents. Air pollution plays a significant role in airborne diseases which is linked to asthma. Pollutants are said to influence lung function by increasing air way inflammation. Alongside pollutants, tobacco smoke increases the risk of attracting these diseases. Many common infections can spread by airborne transmission at least in some cases, including: Anthrax (inhalation), Chickenpox, Influenza, Measles, Smallpox, and Tuberculosis. Airborne diseases are most commonly seen in unsanitary household conditions and overcrowded areas. Also, these diseases thrive in areas of poverty and poor hygienic conditions. Tuberculosis (TB) happens to be one of the most leading causes of death in adults from infectious diseases. Around 95 percent of people suffering from this disease are from developing areas in the world. Measles and diphtheria are two diseases found in poverty conditions, but over the years these diseases have been eliminated due to vaccines in developed countries. Airborne diseases can also affect non-humans. For example, New Castle Disease is an avian disease that effects many types of domestic poultry worldwide which is transmitted via airborne contamination. Often, airborne pathogens or allergens cause inflammation in the nose, throat, sinuses, and the upper airway lungs. Upper airway inflammation causes coughing congestion,and sore throat. This is caused by the inhalation of these pathogens that affect a person's respiratory system or even the rest of the body. Sinus congestion, coughing and sore throats are examples of inflammation of the upper respiratory air way due to these airborne agents.
Causes of Airborne Diseases:
Airborne Diseases are caused by pathogenic microbes small enough to be discharged from an infected person via coughing, sneezing, laughing and close personal contact or aerosolization of the microbe. The discharged microbes remain suspended in the air on dust particles, respiratory and water droplets. Illness is caused when the microbe is inhaled or contacts mucus membranes or when secretions remaining on a surface are touched. Transmission of airborne diseases can be greatly reduced by practicing social and respiratory etiquette. Staying home when ill, keeping close contact with an ill person to a minimum, allowing a few feet distance from others while ill, and wearing a mask, covering coughs and sneezes with elbow or tissue can greatly reduce transmission. Good hand washing can decrease spread of germ-containing droplets that could be picked up on hands from surfaces or hand contact with secretions. Environmental controls and engineering alternatives help reduce transmission of water droplet aerosolized pathogens.
About Airborne Disases:
Airborne Infection Control utilizing MICROCON Mobile Hospital Negative Pressure Rooms Air Purification Systems: Many of these diseases require prolonged exposure for infection to occur, posing only minimal threat to emergency responders. However, there are preventive measures, such as wearing masks or maximizing ventilation, that help reduce these risks. As one can clearly see above on this page maximizing ventilation procedures and airflow circulation procedures are the very crux and heart of our MICROCON 800/400 series.
Applications for Airborne Infection Control in Hospitals and Health Care (healthcare) Facilities
Negative Pressure Isolation Rooms for treatments of patients infected with Tuberculosis TB, H1N1 Swine Flu, H5N1 Avian Bird Flu.
Create or Convert Rooms:
- Negative Air Pressure Isolation Rooms
- Negative Pressure Ventilation Isolation Rooms
- Architects AAI Negative Pressure Hospital HVAC Systems
- AIR Airborne Isolation Room
- AIIR Airborne Isolation Rooms
Positive Pressure Isolation Rooms for treatments of patients infected with HIV Patients and Bone Marrow Transplants
Create or Convert Rooms:
- Positive Air Pressure Isolation Rooms
- Positive Pressure Ventilation Isolation Rooms
- Architects AAI Positive Pressure Hospital HVAC Systems
- AIR Airborne Isolation Room
- AIIR Airborne Isolation Rooms
Epidemiology Infection Control
- Airborne Infectious Diseases
- Airborne Infection Isolation
- Infection Control Healthcare Workers
Other Diseases subject to Negative Pressure Isolation Rooms
- Diphtheria
- Type M TB Tuberculosis
- MDR TB Tuberculosis
- Measles
- Varicella (Chickenpox) including disseminated Herpes Zoster
- Rubella
- Pertussis
- Mumps
- Invasive N Meningitidis Disease
- Invasive H Influenza Disease
AIRBORNE PRECAUTIONS
To reduce the risk of airborne transmission of infectious agents. Hospitals, Health Care Workers, and Care Takers should use Airborne Precautions for patients known or suspected to have infection s transmitted by droplet nuclei (particles 5 microns or smaller in size). Illnesses include: Type M Tuberculosis, Measles, Varicella (Chickenpox), including disseminated Zoster.
Patients must be placed in a negative air pressure isolation room providing the ventilation to prevent transmission of droplet nuclei. Without negative pressure ventilation, infectious droplet nuclei can remain suspended in air for long periods of time.
Doors and windows in negative pressure isolation rooms must be kept closed at all times. Hospital personnel and visitors entering an Airborne Isolation Room (AIR) must wear the N95 TB respirator.
For patients isolated with chickenpox or measles persons immune to chickenpox or measles may enter an Airborne Isolation Room (AIR) without a mask. Patients in a Airborne Isolation Room (AIR) must remain in their room. Patients should leave their room only for essential studies. Patients must wear a paper surgical mask when leaving their room.
GUIDELINES FOR INFECTION CONTROL and INFECTION CONTROL ISOLATION SYSTEM DROPLET PRECAUTIONS
To reduce the risk of droplet transmission of infectious agents. Involves contact of the conjunctivae, or mucous membranes of the nose or mouth of a susceptible person with large droplets (greater than 5 microns in size) containing microorganisms from a person who has clinical disease or is a carrier of the microorganism.
Illnesses include: Diphtheria, Type M TB Tuberculosis Influenza, Rubella, Pertussis, Mumps, Invasive N. meningitidis disease, Invasive H. influenzae disease, etc.
Droplets are generated during sneezing, coughing, talking, and during certain procedures such as suctioning or bronchoscopy.
Close contact (usually 3 feet or less) to the infectious person is required for transmission of the disease. Large droplets travel only short distances and do not remain suspended in the air.
Hospital personnel and visitors entering a Droplet isolation room must wear a paper surgical mask.
RESOURCES:
CDC Hospital Infection Control in Hematopoietic Stem Cell Transplant Recipients "HSCT" http://www.cdc.gov/ncidod/eid/vol7no2/dykewicz.htm
CDC Interim Guidance on Infection Control Measures for 2009 H1N1 Influenza in Healthcare Settings, Including Protection of Healthcare Personnel http://www.cdc.gov/h1n1flu/guidelines_infection_control.htm
MICROCON® US Patent 5,240,478
Please feel free to download our whole catalog
so you can print this out and have your own personal copy.
Click download
to begin downloading a copy of our products catalog.
How
HEPA Filters Work to Control Airborne Pathogens
(from the November 1997 Issue of "Infection Control Today" by
Gary D. Messina)
"High-Efficiency
Particulate Air (HEPA) filter: a specialized
filter that is capable of removing 99.97% of
particulates 0.3 microns in diameter and that
may assist in controlling the transmission of Mycobacterium
tuberculosis." That's the CDC
definition of a HEPA filter. But why has this
type of filter proven to be so effective for
so many decades, and why is it so indispensable
in applications ranging from the nuclear industry
to the electronics, pharmaceutical, and healthcare
fields?
|
|
HEPA filters have
been recognized in the CDC Guidelines for the Prevention
and Transmission of TB in Health Care Facilities to
play an important role in the containment of airborne
infectious pathogens. However, what principles or collection
mechanisms are utilized and applied that can allow
a tiny particle, such as M. tuberculosis, an
airborne pathogen that is rod shaped and 0.4 - 1.4
microns in size, to be effectively captured by a HEPA
filter or, for that matter, any bacteria, mold spore,
fungi, or microbe?
HEPA Media
The heart of any HEPA filter lies in the media
and the fiber formulation. The media or matrix is comprised
of a blend of 100% micro-glass (vitreous) fibers of various
diameters that are randomly dispersed in a filter mat
and bonded together with acrylic resin binders, water
and chemicals in a wet-laid process. The binder provides
the strength for the fibers to allow for filter fabrication,
such as pleating. These man made micro-glass fibers are
unique in their cylindrical shape; they are straight
and uniform in diameter. Higher percentages of fine diameter
glass fibers in the media yield higher media filter efficiencies.
These precise formulas of ingredients and the exact process
control of the formulations yield duplicable physical
characteristics of product. This is one reason HEPA filters
are so consistently uniform in their performance.
 |
Figure
1:
HEPA filter magnified
500 times. |
Figure 1 is a photograph
of what the HEPA filter media looks
like when magnified 500 times. The fibers being randomly
dispersed create a very tortuous path for the air to
follow. You can observe there is no controlled pore
size and various fiber diameters are attached to each
other by the binder. This irregular pathway through
this maze of vitreous fibers allows for depth loading
and capture of the smallest of particulates. The reason
that HEPA filters cannot be cleaned out and reused
is because the captured particles are bound to the
fibers.
Filters are measured
by efficiency levels and efficiencies are only relevant
when compared to a particular particle size. For example,
a filter can claim to be 100% efficient, but to what? Chicken
wire is 100% efficient on chickens, but 0% on flies.
The point being that you always need to relate efficiency
to particle size.
HEPA filters have a minimum efficiency of 99.97% on particles 0.3 microns
in size or larger. The most widely recognized standard test method for
HEPA filters uses 0.3 thermally generated DOP particles as a challenge
agent and is based upon this size being viewed as the most penetrating
particle size and being near the minimum efficiency level and therefore
efficiency will be greater for all other sizes. As a comparison, the
diameter of a human hair measures 75 microns across, we're talking about
pretty small stuff, particle sizes that are invisible to the naked eye.
To understand the
efficiency level of a HEPA that is 99.97%, means that
for every 10,000 particles .3 microns in size or larger
that are challenged by the filter, only 3 particles
will not be captured. HEPA filters are also available
in 99.99% and 99.999% efficiency levels, but 99.97%
on 0.3 microns defines a HEPA. The testing and certification
of HEPA filters is another topic all together, but
HEPA filters with penetration levels above .030% do
not qualify, and all HEPA filters must be individually
tested and certified by prescribed industry and federal
standards.
HEPA Efficiency
HEPA filters never become less efficient than
their initial efficiency rating (unless damaged). It
is sometimes a misunderstanding that these filters need
to be replaced, because they have lost their efficiency.
HEPA filters actually increase in efficiency as they
become loaded because the tiny particles continually
build up and the entrapped particles act as tiny filters.
Operating HEPA filters at lower air flow velocities will
also improve efficiency levels. HEPA's need replacement
because they load up with contaminates which gradually
decrease airflow and increase resistance (delta P) to
a point that maintaining a prescribed cfm becomes diminished.
That is why pressure sensing devices are utilized, which
are a measure to determine filter life.
Now that we have
outlined what makes a HEPA filter and what determines
a HEPA filter, we will look at why HEPA filters are
so efficient.
Technology
of Capture
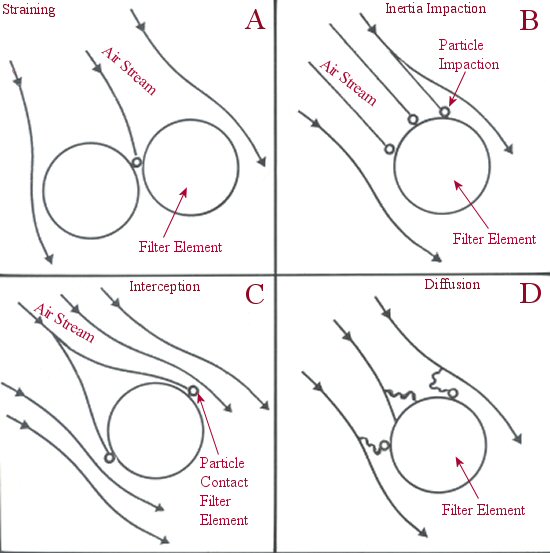
HEPA filters use four different capture mechanisms.
Straining or sieving is the easiest to understand because
it provides a simple principal (Figure 2-A). The object
is larger than the opening through which it can pass and,
therefore, it comes to a barrier and is stopped. Due
to the physical fiber matrix structure of the filter
media, this principal of filtration decreases the life
expectancy of a HEPA as these larger particles tend to
clog up the pathways and cause surface loading. Prefilters
are usually used to filter out the large particulate,
allowing the HEPA to contain the smaller particles, the
purpose for which it was designed
Inertia Impaction
Inertia impactment or impingement is very effective
for particles usually larger than one micron in size
(Figure 2-B). These larger size particles are a mass
in an air stream and collide with the fibers in the fiber
media head-on. They are large enough not to be able to
maneuver or travel around the fiber bed, so they become
impaled and entrapped on the fiber through a collision.
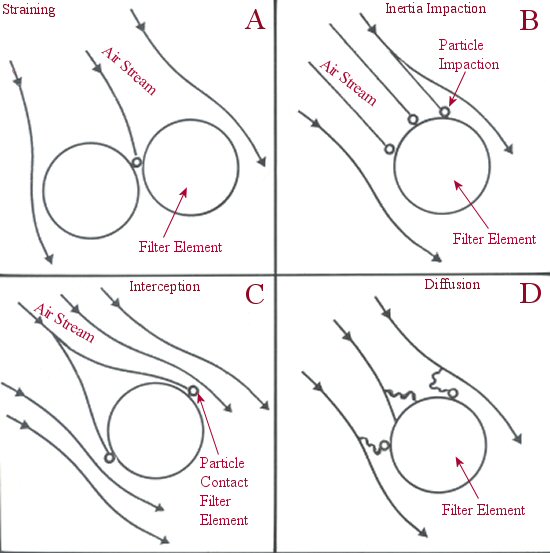
Figure 2: HEPA
filters use four different capture mechanisms: A-straining,
B-inertia impaction,
C-interception, and D-diffusion.
Interception
Interception is very effective on particles larger
than 0.1 micron in size (Figure 2-C). As these lightweight
particles travel in the air stream, they will flow around
a fiber or obstruction. When they make contact with a
fiber, the particle is captured. The bonding or attraction
to the particles to the fiber is due to an intermolecular
surface adhesion known as van der Wael's forces.
Diffusion
The final capture mechanism is known as diffusion
or Brownian Motion (Figure 2-D). Particles that are smaller
than 0.1 micron in size are bombarded by air molecules.
In 1827, Robert Brown, a Scottish botanist, reported
on small particles called molecules. These molecules
were in a continually random motion. As a result of this
motion, particles migrated from areas of high concentration
to areas of low concentration, a process called diffusion.
As the molecules collide with airborne submicron size
particles, they create a spontaneous intermingling. This
causes them to travel in an erratic path within the air
stream (Brownian Movement), thereby improving their chances
of colliding with the filter fibers, at which point they
are retained by the intermolecular van der forces. Diffusion
is a result of velocity. The lower the air flow
velocity, the greater the possibility of a particle colliding
with the fibers. This approach, therefore, works even
when the space between the fibers may be larger than
the captured particle. Particles more than one micron
in size have virtually no effect on this capture mechanism.
The relation of inertia to interception/diffusion is
based not only on particle size retention, but airflow
velocity. Inertia is based on high-velocity impaction
of the particle, while the others depend on lower velocities.
Filter efficiency increases with decreasing particle
size and decreases with the increase of air velocity.
Conclusion
When it comes to airborne infection control,
the HEPA filter is a highly effective, reliable, refined,
and dependable airpurification device. It has proven
its worth for protection of individuals, property, and
process in countless applications throughout the world
for more than 40 years. There are virtually no restrictions
or cautions as to its use. Humidity, heat, cold, component
exposure, or creating ideal operational conditions for
its optimum use play no part in its effectiveness. HEPA
filters improve with use, most other systems deteriorate
with continued use. Improvements to the filter components,
materials, and testing procedures continue unabated in
a variety of industries. Efficiency levels for HEPA filters
reach 99.97% on 0.3 micron, and for ultra-low penetration
air (ULPA) filters as high as 99.9999999% on 0.12 micron.
Like any device, it needs to be properly installed, maintained,
and correctly applied. Beyond the healthcare field,
the electronics industry would cease to exist without
the ability to create particulate-free, controlled environments
with the HEPA filter as its heart.
|
|